Cancer Sufferers Face Unsightly Delays in Remedy Approvals
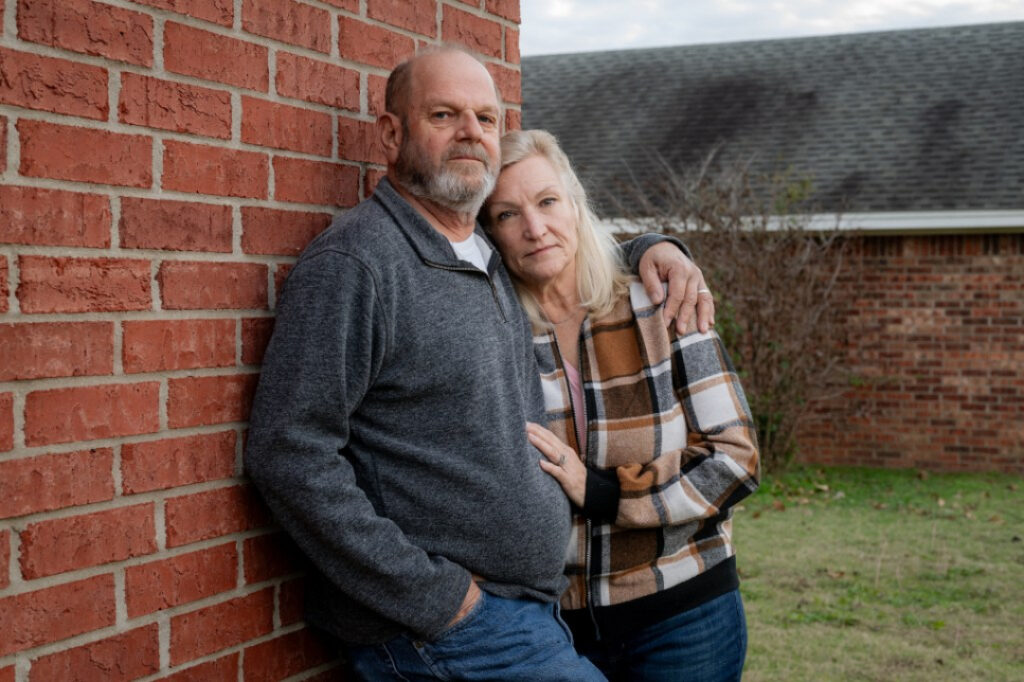
Marine Corps broken-down Ron Winters clearly remembers his doctor’s sobering evaluation of his bladder most cancers evaluation in August 2022.
“That is flawed,” the 66-year-veteran Durant, Oklahoma, resident remembered his urologist pronouncing. Winters braced for the wrestle of his existence.
Exiguous did he await, however, that he wouldn’t be waging battle finest against most cancers. He also modified into up against the Department of Veterans Affairs, which Winters blames for dragging its feet and organising obstacles which procure delayed his therapies.
Winters didn’t undergo most cancers medication at a VA facility. As an replacement, he sought care from a specialist during the Veterans Health Administration’s Neighborhood Care Programestablished in 2018 to enhance veterans’ picks and reduce their wait instances. But he acknowledged the prior authorization project modified into a chronic nightmare.
“For them to take weeks — up to months — to produce an authorization is ridiculous,” Winters acknowledged. “It doesn’t topic if it’s most cancers or not.”
After his initial evaluation, Winters acknowledged, he waited four weeks for the VA to approve the plot that allowed his urologic oncologist at the University of Texas Southwestern Scientific Heart in Dallas to remove one of the crucial most most cancers. Then, when he accomplished chemotherapy in March, he modified into compelled to wait yet every other month while the VA thought to be approving surgical treatment to remove his bladder. Even routine imaging scans that Winters needs each 90 days to trace growth require preapproval.
In a written response, VA press secretary Terrence Hayes acknowledged that a “prolong in care isn’t very acceptable.” After KFF Health News inquired about Winters’ case, the VA began working with him to derive his ongoing care authorized.
“We are in a position to also urgently evaluation this topic and take steps to effect sure it does not happen again,” Hayes educated KFF Health News.
Prior authorization isn’t uncommon to the VA. Most non-public and federal smartly being insurance packages require patients to derive preapprovals for sure therapies, assessments, or prescription medicines. The project is supposed to diminish spending and keep a ways from unnecessary, ineffective, or duplicative care, even supposing the stage to which companies and companies discipline these rules varies.
Insurers argue prior authorization makes the U.S. smartly being care machine extra efficient by cutting extinguish — theoretically a get for patients who will likely be harmed by excessive or futile medication. But critics inform prior authorization has change loyal into a machine that insurers employ to restrict or prolong costly care. It’s an particularly alarming subject for folk identified with most cancers, for whom suggested medication can mean the inequity between existence and death.
“I’m attracted to brand and affordability,” acknowledged Fumiko Chino, a member of the Affordability Working Community for the Memorial Sloan Kettering Cancer Heart. But the style prior authorization is used now enables insurers to implement “denial by prolong,” she acknowledged.
Electronic mail Ticket-Up
Subscribe to KFF Health News’ free Morning Briefing.
Cancer is one of perhaps the costliest categories of disease to treat in the U.S., in step with the Centers for Illness Adjust and Prevention. And, in 2019, patients spent higher than $16 billion out-of-pocket on their most cancers medication, a picture by the Nationwide Cancer Institute found.
To effect matters worse, many most cancers patients procure had oncology care delayed attributable to prior authorization hurdles, with some facing delays of upper than two weeks, in step with examine Chino and colleagues published in JAMA in October. One other present perceive found that indispensable insurers issued “unnecessary” initial denials in line with imaging requests, most fundamentally in endocrine and gastrointestinal most cancers instances.
The federal govt is weighing fresh rules designed to present a enhance to prior authorization for thousands and thousands of oldsters lined by Medicare, Medicaid, and federal marketplace plans. The reforms, if appliedwould shorten the length insurers are permitted to procure in mind prior authorization requests and would also require companies to produce extra knowledge when they subject a denial.
For the time being, patients — rather a pair of whom are facing the worst evaluation of their lives — must navigate a machine marked by roadblocks, crimson tape, and appeals.
“That is cruel and peculiar,” acknowledged Chino, a radiation oncologist. A two-week prolong will likely be lethal, and that it continues to happen is “unconscionable,” she acknowledged.
Chino’s examine has also proven that prior authorization is straight related to elevated apprehension among most cancers patients, eroding their have faith in the smartly being care machine and wasting each the provider’s and the affected person’s time.
Leslie Fisk, 62, of Recent Smyrna Sea traipse, Florida, modified into identified in 2021 with lung and mind most cancers. After seven rounds of chemotherapy final year, her insurance company denied radiation medication advised by her clinical doctors, deeming it medically unnecessary.
“I endure in mind shedding my mind. I would like this radiation for my lungs,” Fisk acknowledged. After battling Florida Health Care Plans’ denial “tooth and nail,” Fisk acknowledged, the insurance company relented. The insurer did not answer to requests for reveal.
Fisk called your whole project “horribly demanding.”
“You’ll need to navigate perhaps the most refined machine in the sector,” she acknowledged. “In case you’re correct sitting there staring at for them to take care of you, they received’t.”
A fresh KFF picture found that patients who are lined by Medicaid seem to be particularly impacted by prior authorization, despite their smartly being concerns. About 1 in 5 adults on Medicaid reported that their insurer had denied or delayed prior recognition of a medicine, carrier, seek suggestion from, or drug — double the rate of adults with Medicare.
“Patrons with prior authorization complications tend to face other insurance complications,” reminiscent of tension finding an in-network provider or reaching the limit on lined products and services, the picture illustrious. They also are “a ways extra likely to journey excessive smartly being and monetary penalties when put next to other folks whose complications did not absorb prior authorization.”
In some instances, patients are pushing serve.

In November, USA Lately reported that Cigna admitted to making an error when it denied protection to a 47-year-veteran Tennessee lady as she ready to undergo a double-lung transplant to treat lung most cancers. In Michigan, a aged smartly being insurance govt educated ProPublica that the company had “crossed the line” in denying medication for a man with lymphoma. And Blue Rotten and Blue Defend of Louisiana “met its match” when the company denied a Texas trial lawyer’s most cancers medication, ProPublica reported in November.
Endless others procure modified into to social media to shame their smartly being insurance companies into approving prior authorization requests. Regulations has been launched in as a minimum 30 states — from California to North Carolina — to address the inconvenience.
Lend a hand in Oklahoma, Ron Winters is smooth battling. In accordance to his wife, Teresa, the surgeon acknowledged if Ron would perhaps procure passed through his operation sooner, they would perhaps perhaps procure shunned eradicating his bladder.
In many techniques, his story echoes the national VA scandal from almost a decade ago, in which veterans across the country had been languishing — some even demise — as they waited for care.
In 2014, for example, CNN reported on broken-down Thomas Breen, who modified into kept staring at for months to be viewed by a health care provider at the VA in Phoenix. He died of stage 4 bladder most cancers earlier than the appointment modified into scheduled.
Winters’ most cancers has spread to his lungs. His evaluation has stepped forward to stage 4.
“In actuality, nothing has modified,” Teresa Winters acknowledged. “The VA’s processes are smooth broken.”
Manufacture you are going to procure an journey with prior authorization you’d love to portion? Click here to present an rationalization to your story.






